The Future of Physical Therapy: Evidence, Innovation, and the Human Touch
Highlights
• Rehabilitation is a global health priority: demand for high-quality rehab is rising and WHO’s Rehabilitation 2030 initiative calls for integrating rehabilitation across health systems.
• Physical therapy is shifting from “post-injury repair” toward prevention, healthy aging, and performance — professional bodies (e.g., APTA) explicitly promote this vision.
• This post summarizes the best available evidence (systematic reviews, RCTs, professional guidance) and explains how clinics can combine technology and clinical reasoning to deliver future-proof care.

Physical therapy is no longer limited to post-injury recovery. Today, it is at the forefront of prevention, pain management, and healthy aging. Global health authorities, including the World Health Organization, call rehabilitation a priority for the future of healthcare. Forward-looking clinics that integrate research, technology, and patient-centered care are setting the standard. At Al Amal Physical Therapy’s Cairo-based physical therapy clinics, we combine evidence-based rehabilitation and innovative physical therapy approaches to shape the future of physical therapy.
1) The evidence pillars every modern Physical Therapy program must have
Therapeutic exercise remains the bedrock

High-quality reviews show exercise therapy yields clinically meaningful benefits for chronic low back pain and many musculoskeletal conditions; it’s an evidence-based first-line approach.
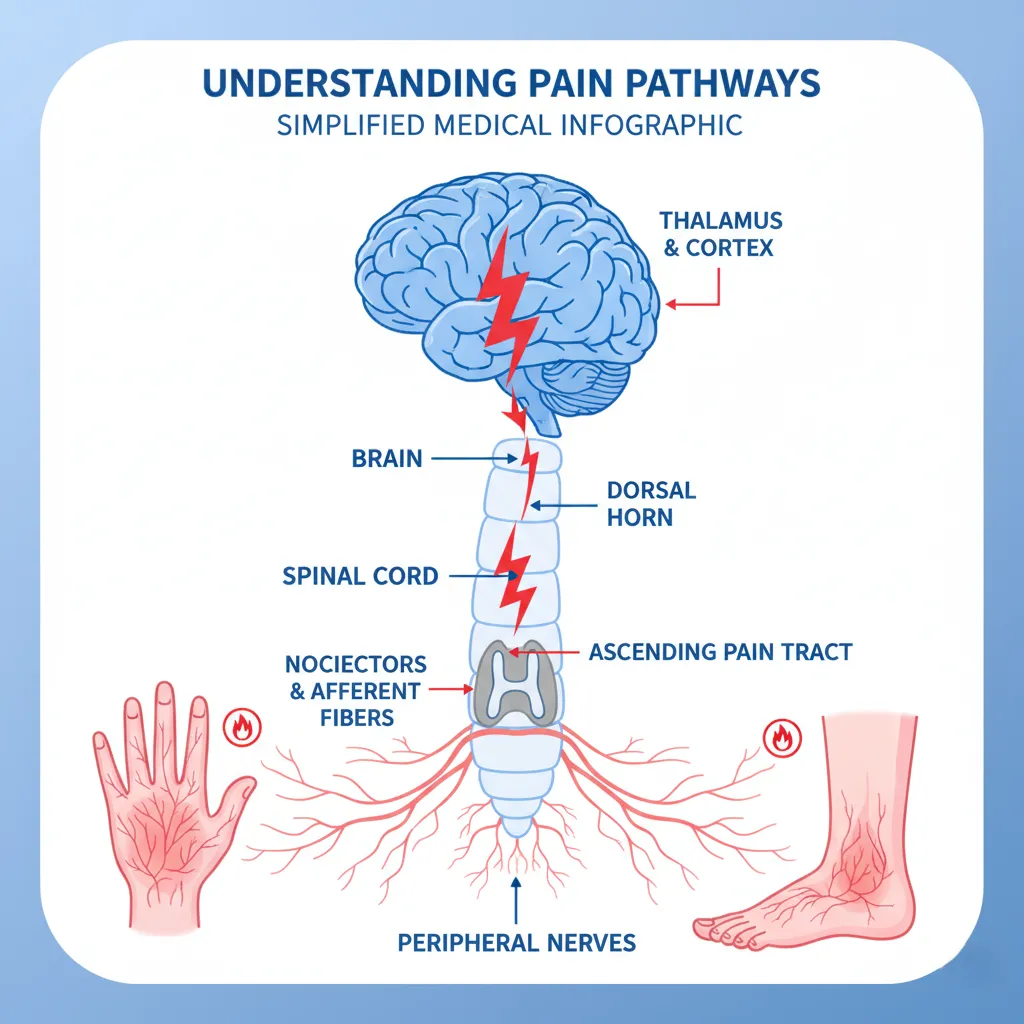
Pain neuroscience education (PNE)

Furthermore, systematic reviews and randomized controlled trials (RCTs) consistently support pain neuroscience education (PNE) for reducing pain, disability, and fear-avoidance, especially when it is integrated into active rehabilitation.
Early physical therapy reduces downstream high-cost care and opioid exposure
Large claims-data analyses and cohort studies show that patients who access physical therapy (PT) early undergo less imaging, receive fewer specialist referrals, and use opioids less over the long term.
Tele-rehabilitation is effective and scalable

Recent systematic reviews and meta-analyses show that Tele-rehab (video visits, guided exercise apps, remote monitoring) delivers outcomes comparable to in-person care for many musculoskeletal and post-operative conditions when designed correctly.
2) Emerging technologies with real evidence
Wearables & consumer sensors “Useful adjuncts, not magic bullets”

Moreover, consumer and clinical wearables provide objective activity and biomechanics data that can enhance adherence and monitoring. However, while current reviews support their adjunctive use, they also emphasize the need for larger randomized controlled trials and cost-effectiveness studies.
AI/computer-vision movement analysis

In addition, camera-based AI can estimate joint angles and gait parameters with sufficient accuracy for many clinical tasks when properly calibrated. However, while validation studies show promising results, they also reveal limitations related to devices and environments for instance, reduced accuracy in ankle kinematics and single-camera setups. Use these tools for objective tracking, remote assessments, and triage — with human oversight.
Robots & exoskeletons

Similarly, robotic gait training and exoskeletons show positive outcomes for patients with subacute stroke and severe gait impairments. However, results vary depending on the device, timing, and training protocol. Therefore, systematic reviews recommend careful patient selection and combining robotic therapy with task-specific training for optimal results.
Regenerative rehabilitation
Moreover, combining rehabilitation science with regenerative medicine including cell and growth-factor therapies as well as tissue engineering represents an active and rapidly evolving research area. Early findings demonstrate biological plausibility and translational potential; however, widespread clinical adoption should await confirmation from high-quality trials and well-defined multidisciplinary pathways.
3) How a top-tier clinic blends evidence + tech + human touch

- Assessment first, data second. By using validated clinical tests + Patient-Reported Outcomes (PROs); add wearable or video assessment to augment (not replace) clinical reasoning.
- Personalized, active programs. Combining exercise, PNE, and behavioral support tools like tele-checkups and app reminders to enhance adherence and achieve better outcomes.
- Early access & triage pathways. Fast referral pathways for acute musculoskeletal (MSK) presentations help reduce downstream costs and minimize opioid exposure.
- Outcome tracking & continuous improvement. Additionally, clinics should track standardized outcome sets such as pain, function, and return-to-work metrics and continuously refine their programs based on aggregated data.
4) Public-facing value (what patients and referrers need to know)

- If you have a new episode of back, neck, knee, or shoulder pain early PT can reduce later imaging, injections, surgeries and opioid use.
- Tele-visits work for many follow-ups and guided home programs; they increase access while maintaining outcomes when combined with structured exercise.
- Education matters: understanding pain (PNE) reduces fear and improves engagement with active rehabilitation.
5) Evidence-based, practical recommendations for clinics
- Offer direct access/fast-track for acute MSK complaints to prioritize early PT.
- Use validated exercise protocols for common conditions (low back, knee OA, shoulder) and pair them with PNE.
- Provide hybrid care: in-clinic baseline + tele-follow-up for progress checks and adherence coaching.
- Use validated wearables or AI-video tools only after local validation with the patient group, document accuracy and limitations publicly.
- Publish patient-facing outcome dashboards (anonymized) to show real-world clinic performance and build trust.
FAQs
Conclusion
Our clinic blends proven therapies (exercise, PNE, early access) with validated digital tools and continuous outcome tracking to deliver safer, more effective, and future-ready care.
Book a fast-track assessment for acute Musculoskeletal pain or ask about our hybrid/research-informed programs.
GET IN TOUCH
Ready to Start Your Journey to Recovery?
References
- Marrache, M., Prasad, N., Margalit, A. et al. Initial presentation for acute low back pain: is early physical therapy associated with healthcare utilization and spending? A retrospective review of a National Database. BMC Health Serv Res 22, 851 (2022). https://doi.org/10.1186/s12913-022-08255-0
- Lin, T. W., Yang, Y., Hong, H. Y., Zhou, X. B., Tung, T. H., Zheng, B. B., & Zhang, J. M. (2025). Effectiveness of telerehabilitation in non-operatively managed shoulder conditions: a systematic review and meta-analysis. BMC musculoskeletal disorders, 26(1), 614. https://doi.org/10.1186/s12891-025-08839-x
- Yang J, Li H, Zhao H, et alEffectiveness of telerehabilitation in patients with post-COVID-19: a systematic review and meta-analysis of randomised controlled trialsBMJ Open 2024;14:e074325. doi: 10.1136/bmjopen-2023-074325
- Latif A, Al Janabi HF, Joshi M, et alUse of commercially available wearable devices for physical rehabilitation in healthcare: a systematic reviewBMJ Open 2024;14:e084086. doi: 10.1136/bmjopen-2024-084086
- Ino, T., Samukawa, M., Ishida, T., Wada, N., Koshino, Y., Kasahara, S., & Tohyama, H. (2023). Validity of AI-Based Gait Analysis for Simultaneous Measurement of Bilateral Lower Limb Kinematics Using a Single Video Camera. Sensors (Basel, Switzerland), 23(24), 9799. https://doi.org/10.3390/s23249799
- WHO — Rehabilitation 2030 initiative. Rehabilitation 2030
- APTA — Vision & strategic guidance for the profession. Vision Statement for the Physical Therapy Profession | APTA
FAQs
In fact, for many musculoskeletal and post-operative conditions, tele-rehabilitation can deliver comparable outcomes to in-person care. This is especially true when programs are well-structured and include consistent clinician oversight.
No. AI tools help quantify movement and scale assessment, but clinical reasoning, manual skills, empathy, and individualized decision-making remain human domains. Use AI as an objective adjunct.
Yes, wearables can indeed enhance monitoring and adherence, making them valuable adjuncts to rehabilitation. However, larger randomized controlled trials and thorough economic analyses are still required before they can be widely implemented.
PNE explains how nervous system processing influences pain; when combined with active rehab it improves pain, disability and movement confidence.
Indeed, studies show that starting physical therapy early leads to better long-term outcomes. In particular, early intervention is associated with reduced high-cost care later on and lower long-term opioid use, making early assessment a valuable and cost-effective step in recovery.








